March 2025
Autonomous Coding Market (By Usage: Machine Learning, NLP, Deep Learning; By Mode Of Delivery: Web & Cloud-based, On-Premises; By End User: Hospitals, Clinical Laboratories Logistics & Transportation, Others) - Global Industry Analysis, Size, Share, Growth, Trends, Regional Outlook, and Forecast 2024-2034
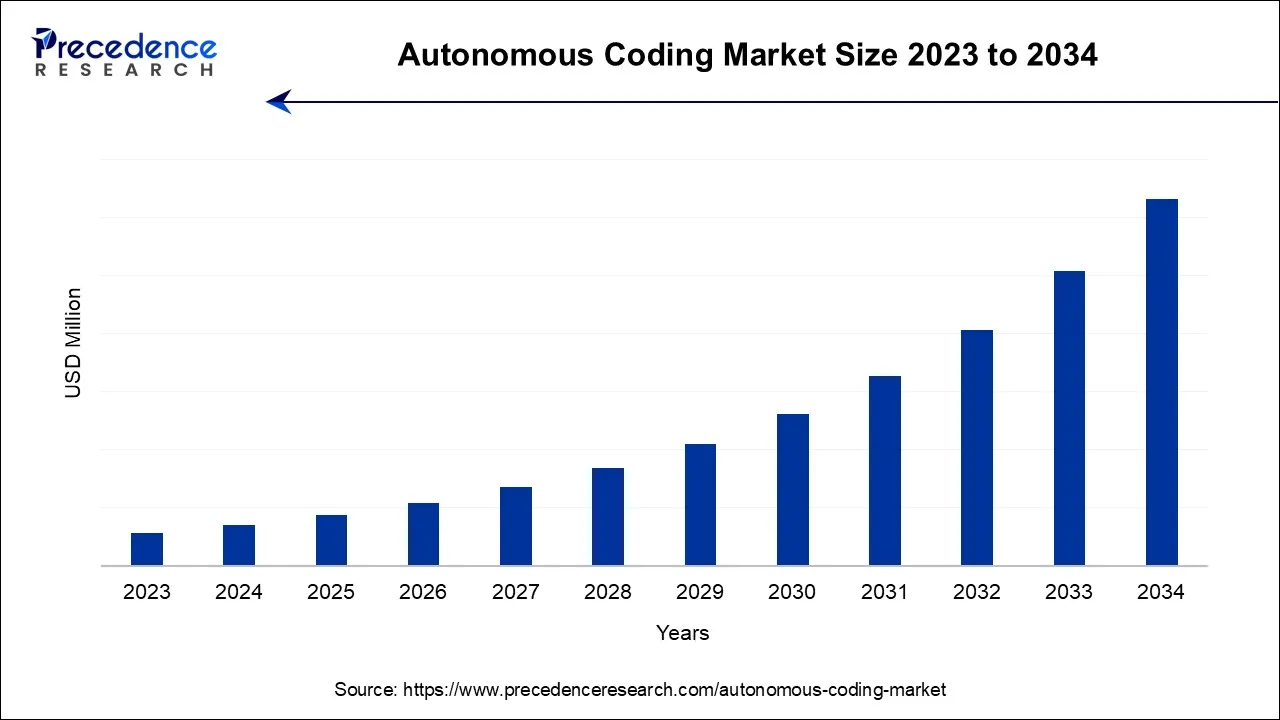
The global autonomous coding market is surging, with an overall revenue growth expectation of hundreds of millions of dollars during the forecast period from 2024 to 2034.
A brand-new and cutting-edge technique called autonomous coding uses a completely automated AI solution to accurately and quickly code charts. Based on cutting-edge clinical language understanding (CLU) technology, autonomous coding is exceptional in its capacity to comprehend freely used medical terminology. CLU is the application of computational linguistics to clinical language along with medical expertise. It enables computers to build models defining the narrative of the doctor's documentation and to comprehend the logical linkages between various linguistic elements in the medical record. Although installing an AI product has several advantages, the primary objective in the medical billing and coding industry is to automate procedures that improve workflow and overall revenue cycle performance.
Productivity and code quality are two key performance indicators (KPIs) that continue to come under close scrutiny. Every clinical element of the medical record is identified by autonomous coding technology. It provides constantly accurate, top-notch medical coding because it comprehends relevancy as well as which codes should be assigned as being the most accurate. Just the charts that the software completely comprehends receive codes. Medical records that are not handled are marked for manual review. Scalable coding services are available from autonomous coding systems without sacrificing precision. Indeed, enormous productivity increases have been made. Medical encounters can be processed by autonomous platforms at a rate of less than five seconds each encounter, with an unlimited capacity. Chart volume fluctuations are handled by simply allocating additional or less computation capacity.
Organizations have been able to overcome coder shortages, streamline the billing process, and lower costs due to the gains in quality and productivity and the system's capacity to operate without human intervention. The audit performance of autonomous coding and its capacity to identify and promptly fix coding problems, without the need to refer encounters back to coders for resolution, are also gaining a lot of attention. Autonomous coding systems offer a transparent audit trail that fully explains the reasoning behind each and every issued code in addition to the recognition improvement.
A speedy validation of the assigned codes is made possible by this technological innovation, which is a byproduct of the fundamental CLU ability to comprehend clinical narrative. It also provides a strong platform for the management of denials and the appeals process. Accounts receivable days (AR), missing charges, and insufficient paperwork all improved for customers who used autonomous coding technology. Moreover, codes are recorded with the utmost level of clarity possible, which has been effective in lowering the number of denials and raising the percentage of clean claims.
| Report Coverage | Details |
| Largest Market | North America |
| Base Year | 2023 |
| Forecast Period | 2024 to 2034 |
| Segments Covered | By Usage, By Mode of Delivery, and By End User |
| Regions Covered | North America, Europe, Asia-Pacific, Latin America, and Middle East & Africa |
Future technological advancements in medical coding are anticipated to occur much more quickly. As the capabilities of artificial intelligence/machine learning (AI/ML) and natural language processing develop, numerous firms are actively looking into the widespread application of autonomous medical coding (AMC). The holy grail of medical coding, a mechanism that can convert clinical data into coded data and receive payment from insurance carriers without requiring human interaction is being developed by organizations using such technologies. AMC systems moreover encourage openness by providing an audit trail of autonomous code. This stage employs a machine learning technique to lessen the likelihood of errors and boost the model's accuracy when the AMC product deals with complex patient interactions.
Programs for medical and billing training require either a high school diploma or a general education development degree as eligibility requirements (GED). This is essential because one will be using very specific medical language. The high school education will provide him/her with the language and math skills they need to succeed in a medical billing and coding training program. So, if they have not earned their GED or completed high school, they do not meet the requirements to participate in a medical billing and coding training programme. If they wish to work as a medical biller and coder, they must finish an approved training course. There is a program for a certificate, diploma, or associate degree. They can find training programs by consulting community colleges, vocational schools, universities, hospitals, and other organizations that offer healthcare courses. The required training program to become a medical biller and coder may take 7 to 24 months to complete, depending on the type of curriculum they choose.
According to the usage segment, machine learning held the maximum market share in 2023. It is a branch of artificial intelligence that enables machines to learn directly from information, experience, and examples. By learning from examples or data rather than by following pre-programmed rules, machine learning enables computers to perform certain jobs intelligently and allows them to carry out complex procedures. Market expansion is being driven by advancing technology advancements that increase system accuracy. Humans interact with a range of machine learning-based systems, such as recommender systems, speech recognition, and image identification.
The rapid advancement of image recognition technology, which has increased the system's accuracy, has fueled the demand for machine learning in many systems. Due to the inclusion of machine learning in robotics, the machine learning industry has also grown. The quick advancement of sensor technology and materials has resulted in several advancements in robotics. Robots now have a greater ability to contribute to initiatives like autonomous vehicles and drones because to the advancement of machine learning. Also, the market has expanded as a result of an increase in demand for sophisticated robotic systems across a variety of sectors, including healthcare, automotive, electronics, food, and beverage.
By mode, Cloud-based solutions held the maximum market share in 2023. They are a more recent strategy that is mostly used by businesses without the required internal infrastructure. These systems require less money to install. Also, this software does not require internal maintenance, which is perhaps the key factor behind its increasing popularity.
By end users, hospitals held the maximum share. Professionals in revenue cycle and health information management (HIM) face a confluence of challenges as the number of healthcare interactions rises. The availability of skilled coding specialists was limited by pandemic-related volatility as senior professionals left, medical leaves occurred, and other coding specialists changed positions. Healthcare provider organisations are under pressure to produce faster, higher-quality coding outputs in order to ensure revenue integrity, reduce reimbursement recoupments, and increase bottom lines as they recover from two years of uncertain cash flows. A 350-bed hospital's typical revenue cycle is $22 million (an estimated 3-5 percent of revenue). All these factors drive the demand for use of autonomous coding in hospitals.
Due to technology advances and better healthcare infrastructure in several of the nations in this region, the North American autonomous coding market is anticipated to hold a sizable share over the projected period. The region's market is expanding as a result of increasing demand for coding services and the high demand for streamlining hospital billing operations due to the rise in chronic diseases, as well as strategic moves made by industry participants in the area.
The market is expanding in part due to the rising prevalence of chronic diseases in the various nations in the region. For instance, according to the American Cancer Society, there will be 1,918,030 new cancer cases in the United States in 2022, which will increase the need for streamlining. The market's growth is also being fueled by the strategic actions made by the market's participants. For example, in October 2022, Canadian company WELL Health Technologies Inc. signed a contract to buy Cloud Practice Inc. and three clinics from CloudMD Software & Services Inc. RBC purchased MDBilling.ca, a cloud-based platform that streamlines and automates medical billing for Canadian doctors, in October 2022.
There are both small and major enterprises in the intensely competitive global market for dental anaesthesia. To boost their market position and increase their market share, these companies have implemented crucial business strategies, such as joint ventures, strategic alliances & partnerships, product innovation, new product launches, and contracts.
Segments Covered in the Report
By Usage
By Mode Of Delivery
By End User
By Geography
For inquiries regarding discounts, bulk purchases, or customization requests, please contact us at sales@precedenceresearch.com
No cookie-cutter, only authentic analysis – take the 1st step to become a Precedence Research client
March 2025
October 2024
November 2024
October 2024