October 2024
AI in Revenue Cycle Management Market (By Type: Integrated, Standalone; By Component: Hardware, Software, Services; By Deployment Mode: Cloud, On-premises; By Application: Patient Scheduling, Eligibility and Benefits Verification, Patient Payment/Timing Estimation, Prior Authorization, Pre-billing Audits, Denials Management, Compliance Monitoring, Fraud Detection, Others; By End User) - Global Industry Analysis, Size, Share, Growth, Trends, Regional Outlook, and Forecast 2024-2034
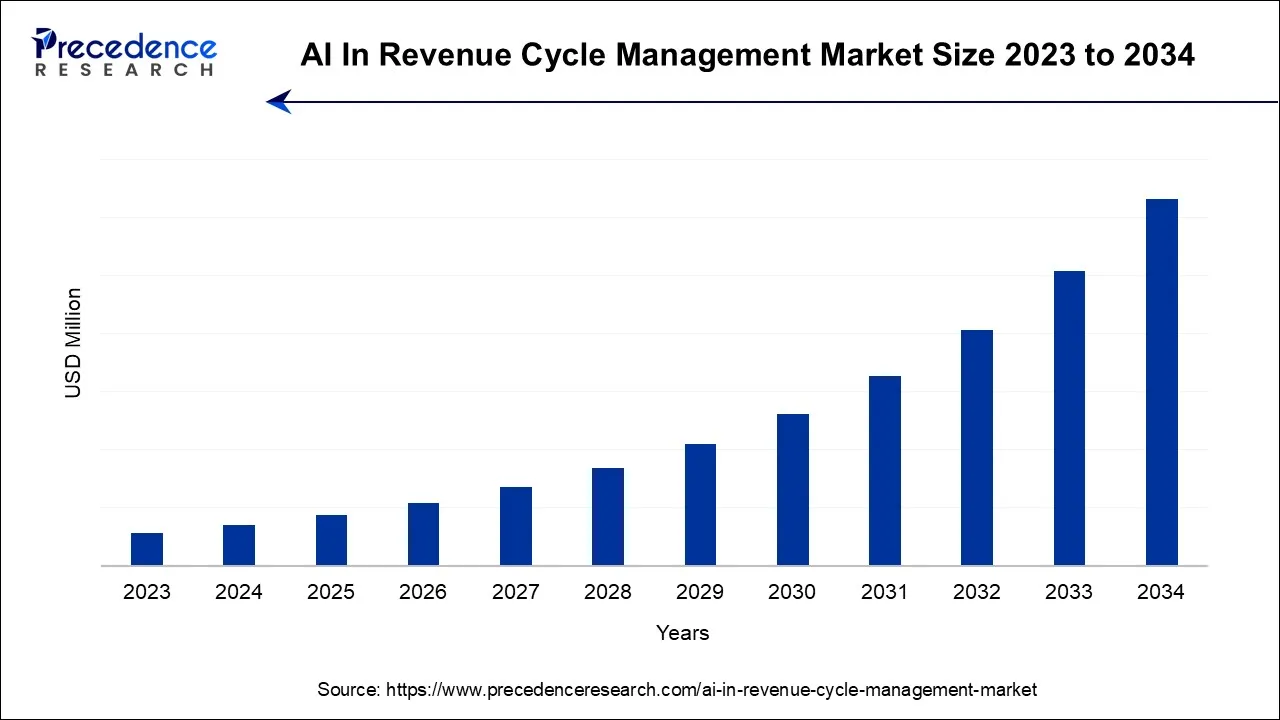
The global AI in revenue cycle management market is surging, with an overall revenue growth expectation of hundreds of millions of dollars during the forecast period from 2024 to 2034.
The use of AI in revenue cycle management (RCM) is revolutionizing the way healthcare organizations manage their financial operations. RCM encompasses the entire process of tracking and managing a patient’s financial interactions within a healthcare provider, from initial appointment scheduling to billing and payment collection. AI technologies are being applied to various stages of this cycle to optimize efficiency, reduce errors, and improve financial outcomes for healthcare providers.
According to the study by Change Healthcare, 655 of all respondents said they are now using AI in RCM (compared to 89% of those who hold RCM jobs). A tech evaluation of AI technology suppliers, solutions, or software systems targeted at enhancing RCM processes and 98% of healthcare leaders expect to use AI in RCM by 2023.
The AI in revenue cycle management market has experienced significant growth in recent years, driven by the increasing complexity of healthcare reimbursements, rising healthcare costs and the need for healthcare providers to improve their financial performance.
AI technologies, including machine learning, natural language processing, and predictive analytics, are being deployed to streamline RCM processes, enhance revenue capture, reduce administrative burdens, and mitigate compliance risks.
| Report Coverage | Details |
| Largest Market | North America |
| FGastest Growing Market | Asia Pacific |
| Base Year | 2023 |
| Forecast Period | 2024 to 2034 |
| Segments Covered | By Type, By Component, By Deployment Mode, By Application, and By End User |
| Regions Covered | North America, Europe, Asia-Pacific, Latin America, and Middle East & Africa |
Patients can get assistance from AI-powered chatbots and virtual assistants with their queries about insurance coverage, payment schedules, and billing. These AI technologies can offer individualized, on-demand support, enhancing patients’ satisfaction and minimizing the workload for employees. RCM employees can complete other activities more quickly due to AI. The team may now access accounts and cases that they might not have had time to explore without the assistance of AI. Thus, the benefit of integrating AI in RCM is expected to influence the market growth over the forecast period.
Healthcare institutions handle a variety of critical and sensitive data, including sensitive patient information. Undoubtedly, they must make sure that data is secure and confidential. Healthcare executive's main worry about integrating AI into their system is data security and privacy. Thus, data privacy and security concerns are expected to be a major restraining factor for AI in the revenue cycle management market during the forecast period.
The increasing acquisitions in the revenue cycle management market are expected to offer a lucrative opportunity for market growth over the forecast period. For instance, in June 2022, the previously announced purchase of Cloudmed was finalized, according to the press release published by R1 RCM Inc., a leading supplier of technology-driven solutions that improve patient satisfaction and healthcare provider's financial performance.
Through the acquisition, the businesses will be in a position to provide a top revenue cycle management platform for healthcare providers and advance digital transformation with the integration of AI. In addition, the company will improve its position in healthcare providers and physician groups owing to its significant experience and solutions that cover the RCM spectrum. Therefore, this kind of strategy adopted by the market players will further boost the market revenue growth over the anticipated timeframe.
Based on the type, the global AI in the revenue cycle management market is segmented into integrated and standalone. The standalone segment is expected to dominate the market during the forecast period. The standalone AI in revenue cycle management offers independent and dedicated AI solutions tailored specifically for optimizing and automating RCM processes within healthcare organizations. These standalone solutions are designed to be integrated seamlessly into existing RCM systems, electronic health records, or other healthcare IT infrastructure. Thus, this is expected to drive the market growth during the forecast period.
Based on the component, the global AI in revenue cycle management market is segmented into hardware, software and services. The software segment is expected to hold a prominent market share over the forecast period. This is attributed to the software used to reduce administrative expenses and stop healthcare fraud. An increasing amount of data has also aided in the adoption of solutions in recent years as a result of the digitization processes and streamlining to improve patient care; as a result, software solutions are being used more frequently and are gaining pace. Thus, this is expected to propel the segment growth over the forecast period.
Based on the deployment mode, the global AI in revenue cycle management market is segmented into cloud and on-premises. The cloud segment is expected to grow at the highest CAGR over the forecast period. The integration of cloud computing into the AI in revenue cycle management market has brought significant advantages to healthcare organizations. Cloud-based AI solutions offer scalability, flexibility, accessibility, and cost-effectiveness, making them an attractive option for optimizing RCM processes. Moreover, the increasing collaboration in the cloud-based RCM industry is also propelling the segment expansion.
Based on the application, the global AI in the revenue cycle management market is segmented into patient scheduling, eligibility and benefits verification, patient payment/timing estimation, prior authorization, pre-billing audits, denials management, compliance monitoring, fraud detection and others. The eligibility and benefits verification segment is expected to hold the largest market share over the forecast period. Verifying benefits and eligibility is the most popular application of AI in RCM in healthcare. It can assist organizations in automatically determining a patient’s eligibility before any claims are made. The most cutting-edge AI businesses are investigating the possibility of contacting insurance companies directly using chatbots and related technology.
Chatbots might offer the most recent patient data that insurance companies might require to assess eligibility. AI systems can enhance accuracy and efficiency by using machine learning algorithms to learn from past data, hence requiring less user involvement. Thereby, driving the segment growth.
Based on the end user, the global AI in revenue cycle management market is segmented into hospitals, physicians, diagnostics laboratories and others. The hospital segment is expected to dominate the market during the forecast period. AI in revenue cycle management is becoming increasingly important for hospitals as they seek to optimize their financial operations, reduce costs, and enhance patient satisfaction. AI-powered RCM solutions are poised to play a vital role in helping hospitals navigate the complexities of healthcare reimbursement while improving overall financial performance. Thus, this is expected to propel the market expansion.
The U.S. AI in revenue cycle management market from 2024 to 2034, provides a comprehensive overview of the industry, market segmentation based on a variety of criteria, and the current vendor landscape. North America is expected to hold the largest market share over the forecast period. This is due to the presence of major hospitals and specialty care centers in the United States. Healthcare systems have undergone a digital transition as a result of regulatory reforms like the ICD-10 revisions, and there has been a sharp increase in demand for healthcare IT solutions like RCM systems to boost productivity and improve service delivery.
Additionally, the region's market is presented with significant development prospects due to the existence of well-established healthcare facilities and favorable laws. Furthermore, the presence of major market players in the region is expected to propel the market growth in the region.
Asia Pacific is Expected to Grow at the Fastest Rate Over the Forecast Period
The market growth in the region is attributed to the growing healthcare infrastructure investment. For instance, according to the report published by NITI Ayog, the healthcare sector in India has been expanding at a CAGR of over 22%. Moreover, substantial government support for the advancements in healthcare sector also promotes market growth in Asia Pacific. Thus, the aforementioned stats drive the market growth in the region.
Market Segmentation
By Type
By Component
By Deployment Mode
By Application
By End User
By Geography
For inquiries regarding discounts, bulk purchases, or customization requests, please contact us at sales@precedenceresearch.com
No cookie-cutter, only authentic analysis – take the 1st step to become a Precedence Research client
October 2024
January 2025
February 2025
February 2025